Herniated Disc
A herniated disc occurs when the soft inner material pushes through the outer disc wall, potentially pressing on nearby nerves. While often painful, most cases improve with proper treatment and time.
Experiencing symptoms of a herniated disc?
Schedule a consultation with Dr. Marc Greenberg to explore minimally invasive options.
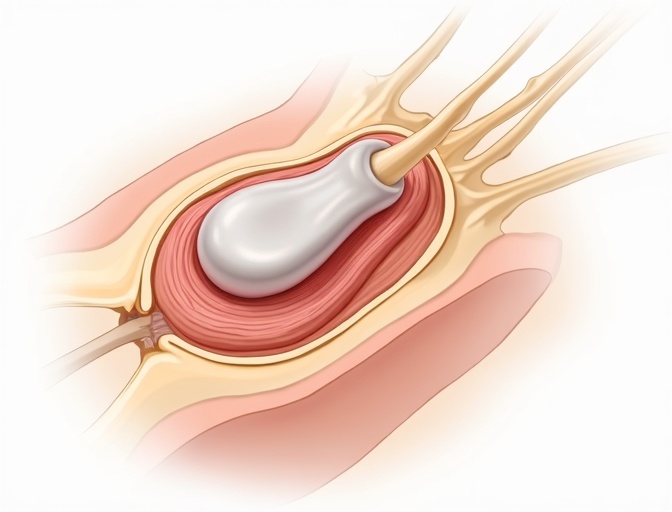
A herniated disc happens when the gel-like center of a spinal disc pushes through a crack in the tough outer layer. This can irritate nearby nerves, causing pain that may travel down your arm or leg. The good news is that most herniated discs heal naturally over time with the right treatment approach.
At Greenberg Spine, we understand how a herniated disc can disrupt your daily life. Dr. Greenberg, fellowship-trained at Mayo Clinic, Johns Hopkins, and Brown University, specializes in both conservative care and advanced minimally invasive techniques to help you return to the activities you love.
Symptoms
Neck or back pain
Localized pain at the disc level, often worse with movement
Radiating pain
Sharp pain traveling down your arm or leg
Numbness and tingling
Loss of feeling or pins-and-needles sensation
Weakness
Difficulty lifting objects or muscle weakness in affected areas
Pain worse with bending or sitting
Increased discomfort with forward flexion activities
Causes
Disc annulus tears
Cracks in the outer disc wall allow inner material to escape
Degeneration
Age-related wear makes discs more prone to herniation
Lifting and rotation injuries
Improper lifting or sudden twisting movements
Genetics
Family history increases risk of disc problems
Diagnosis
Neurological Exam
Dr. Greenberg performs detailed testing of reflexes, muscle strength, and sensation to identify nerve involvement and determine the affected disc level.
- Reflex testing
- Muscle strength assessment
- Straight leg raise test
MRI as Primary Imaging
MRI provides the clearest view of disc herniations and nerve compression. This is the gold standard for diagnosing herniated discs and planning treatment.
- Detailed soft tissue visualization
- Nerve compression assessment
- Treatment planning guidance
When CT/Myelogram is Used
CT myelogram may be used when MRI is not possible (pacemaker, claustrophobia) or when additional detail about bone structures is needed.
- MRI contraindications
- Bone detail visualization
- Surgical planning
Conservative Treatment
Conservative care is the first line of treatment for most herniated discs. Many patients experience significant improvement without surgery.
Activity Modification
Temporary restrictions on lifting, bending, and prolonged sitting to allow healing
NSAIDs and Medications
Anti-inflammatory drugs and nerve pain medications to reduce symptoms
Physical Therapy and Core Strengthening
Targeted exercises to support the spine and improve flexibility
Epidural Steroid Injections
Targeted injections to reduce inflammation around compressed nerves
Heat and Ice Therapy
Application of heat or cold to manage pain and inflammation
Manual Therapy
Chiropractic care and massage to improve mobility and reduce muscle tension
When to Consider Surgery
Surgery is considered when conservative treatments haven't provided adequate relief after 6-12 weeks, or when there are serious neurological symptoms requiring immediate attention.
Objective Triggers for Surgery
- Progressive neurological deficit
- Intractable radicular pain after 6-12 weeks
- Cauda equina syndrome (emergency)
- Significant functional impairment
Why Greenberg Spine
Our advanced approach combines:
- Robotics for precise navigation
- Endoscopic techniques for minimal tissue damage
- Motion-preserving philosophy
- Outpatient focus for faster recovery
Related Procedures
Recovery Expectations
Conservative Treatment
Most patients improve within weeks with proper conservative care. The body's natural healing process can resolve many disc herniations.
Weeks 1-2
Pain management and gentle movement
Weeks 3-6
Physical therapy and gradual activity increase
Weeks 6-12
Return to normal activities and strengthening
Surgical Recovery
Minimally invasive surgery often provides immediate relief of leg pain, with recovery measured in days to weeks rather than months.
Days 1-7
Rest and wound healing, walking encouraged
Weeks 2-4
Gradual increase in activity, physical therapy begins
Weeks 4-12
Return to work and normal activities
Frequently Asked Questions
Will my disc heal on its own?
Many herniated discs can heal naturally over time. The body's immune system can break down the herniated disc material, and symptoms often improve within 6-12 weeks with conservative treatment.
How long does it take to feel better?
Most patients see improvement within 6-12 weeks with conservative treatment. Surgical patients typically experience immediate relief of leg pain, with full recovery in 2-6 weeks for minimally invasive procedures.
What's the difference between microdiscectomy and endoscopic surgery?
Endoscopic surgery uses a smaller incision (8mm vs 2-3cm) and specialized camera, resulting in less tissue damage and faster recovery. Both are effective, but endoscopic may be preferred for certain disc locations.
Is disc replacement an option for herniated discs?
Disc replacement is typically reserved for degenerative disc disease rather than acute herniations. Most herniated discs are treated with decompression procedures like microdiscectomy or endoscopic surgery.
When can I return to lifting after surgery?
Light lifting (under 10 pounds) typically begins at 2 weeks post-surgery. Full lifting restrictions are usually lifted at 6-12 weeks, depending on the procedure and individual healing.
Ready to Find Relief from Your Herniated Disc?
Schedule a consultation with Dr. Greenberg to explore your treatment options and get back to living pain-free.
Medical Disclaimer: The information provided on this page is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider for proper diagnosis and treatment recommendations. Individual results may vary.
Source: American Association of Neurological Surgeons (AANS) and North American Spine Society (NASS) clinical guidelines.